Molecular classification of ovarian high-grade serous/endometrioid carcinomas through multi-omics analysis: JGOG3025-TR2 study
IF 6.4
1区 医学
Q1 ONCOLOGY
引用次数: 0
Abstract
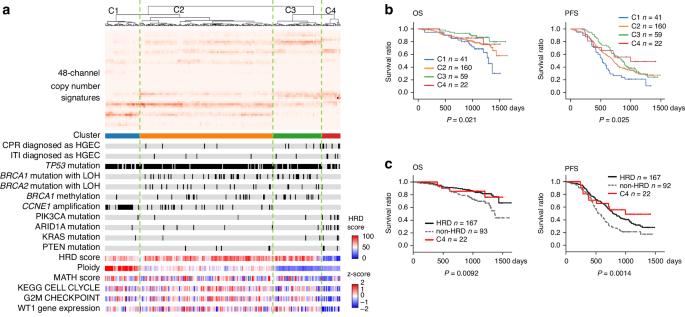
Considerable interobserver variability exists in diagnosis of ovarian high-grade endometrioid carcinoma (HGEC) and high-grade serous carcinoma (HGSC) due to histopathological similarities. While homologous recombination deficiency (HRD) correlates with drug sensitivity in HGSC, the molecular features of HGEC are unclear. Fresh-frozen samples from 15 ovarian HGECs and 274 ovarian HGSCs in the JGOG-TR2 cohort were submitted to targeted DNA sequencing, RNA sequencing, DNA methylation array, and SNP array. We additionally analyzed 555 ovarian HGSCs from TCGA-OV and 287 endometrial high-grade carcinomas from TCGA-UCEC. Unsupervised clustering using copy number signatures identified four distinct tumor groups (C1, C2, C3 and C4). C1 (n = 41) showed CCNE1 amplification and poor survival. C2 (n = 160) and C3 (n = 59) showed high BRCA1/2 alteration frequency with low and moderate ploidy, respectively. C4 (n = 22) was characterized by favorable outcome, higher HGEC proportion, no BRCA1/2 alteration or CCNE1 amplification, and low levels of HRD score, ploidy, intra-tumoral heterogeneity, cell proliferation rate, and WT1 gene expression. Notably, C4 exhibited a normal endometrium-like DNA methylation profile, thus, defined as “HGEC-type” tumors, which were also identified in TCGA-OV and TCGA-UCEC. Ovarian “HGEC-type” tumors present a non-HRD status, favorable prognosis, and endometrial differentiation, possibly constituting a subset of clinically diagnosed HGSCs.

通过多组学分析对卵巢高级别浆液性/子宫内膜样癌进行分子分类:JGOG3025-TR2研究。
背景:由于组织病理学的相似性,卵巢高级别子宫内膜样癌(HGEC)和高级别浆液性癌(HGSC)的诊断存在很大的观察者间差异。同源重组缺陷(HRD)与 HGSC 的药物敏感性相关,但 HGEC 的分子特征尚不清楚:方法:我们对JGOG-TR2队列中的15个卵巢HGEC和274个卵巢HGSC的鲜冻样本进行了DNA靶向测序、RNA测序、DNA甲基化阵列和SNP阵列分析。我们还分析了来自TCGA-OV的555例卵巢高分化干细胞和来自TCGA-UCEC的287例子宫内膜高级别癌:结果:利用拷贝数特征进行无监督聚类,确定了四个不同的肿瘤组(C1、C2、C3 和 C4)。C1(n = 41)表现为CCNE1扩增和生存率低。C2(n = 160)和C3(n = 59)分别显示高BRCA1/2改变频率和低倍体及中等倍体。C4(n = 22)的特点是预后良好,HGEC比例较高,无BRCA1/2改变或CCNE1扩增,HRD评分、倍性、瘤内异质性、细胞增殖率和WT1基因表达水平较低。值得注意的是,C4表现出正常子宫内膜样DNA甲基化特征,因此被定义为 "HGEC型 "肿瘤,这也是在TCGA-OV和TCGA-UCEC中发现的 "HGEC型 "肿瘤:结论:卵巢 "HGEC型 "肿瘤具有非HRD状态、良好的预后和子宫内膜分化,可能是临床诊断的HGSCs的一个子集。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
British Journal of Cancer
医学-肿瘤学
CiteScore
15.10
自引率
1.10%
发文量
383
审稿时长
6 months
期刊介绍:
The British Journal of Cancer is one of the most-cited general cancer journals, publishing significant advances in translational and clinical cancer research.It also publishes high-quality reviews and thought-provoking comment on all aspects of cancer prevention,diagnosis and treatment.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


