Association of Frailty With Clinical and Financial Outcomes Following Liver Transplantation
Abstract
Introduction
Frailty, a measure of physiological aging and reserve, has been validated as a prognostic indicator of mortality in patients with cirrhosis. However, large-scale analyses of the independent association of frailty with clinical and financial outcomes following liver transplantation (LT) are lacking.
Methods
Adults (≥18 years) undergoing LT were identified in the 2016–2020 National Readmissions Database. Frailty was defined using the binary Johns Hopkins Adjusted Clinical Groups frailty indicator. Multivariable linear and logistic regression models were developed to evaluate the independent association of frailty with in-hospital mortality, perioperative complications, and costs.
Results
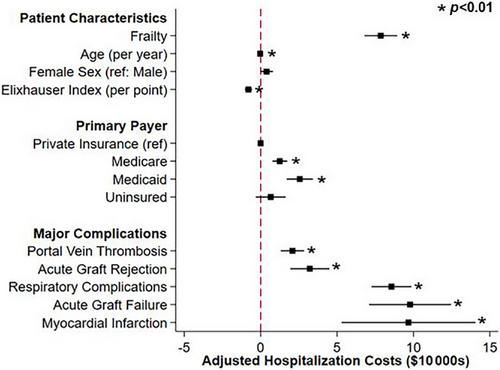
Of an estimated 34 442 patients undergoing LT, 8265 (24%) were frail. After adjustment, frailty was associated with greater odds of mortality (adjusted odds ratio [AOR] 1.80; 95% Confidence Interval [CI]: 1.49–1.18), postoperative length of stay (β + 11 days; 95% CI: +10, +12), and hospitalization costs (+$86 880; 95% CI: +75 660, +98 100), as well as a two-fold increase in relative risk of nonhome discharge (AOR 2.17, 95% CI: 1.90–2.49).
Conclusions
Frailty is associated with an increased risk of in-hospital mortality, complications, and resource utilization among LT recipients. As the proportion of frail LT patients continues to rise, our findings underscore the need for novel risk-stratification and individualized care protocols for such vulnerable patients.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


