Genetic association of serum calcium, phosphate, vitamin D, parathyroid hormone, and FGF23 with the risk of aortic stenosis
引用次数: 0
Abstract
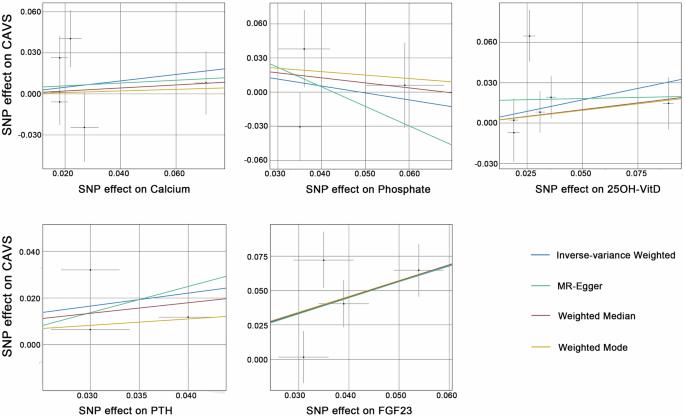
Disorders of mineral metabolism, including elevated levels of serum calcium, phosphate, 25-hydroxyvitamin D (25OH-VitD), parathyroid hormone (PTH), and fibroblast growth factor 23 (FGF23), have been reported in patients with calcific aortic valve stenosis (CAVS). However, evidence of the causal role of mineral metabolism in CAVS is still lacking. In this study, we employed a systematic pipeline combining Mendelian randomization (MR), Steiger directionality test, colocalization analysis, protein-protein network, and enrichment analysis to investigate the causal effect of mineral metabolism on CAVS. Genome-wide association study (GWAS) and protein quantitative trait loci data for mineral metabolism markers were extracted from large-scale meta-analyses. Summary statistics for CAVS were obtained from two independent GWAS datasets as discovery and replication cohorts (n = 374,277 and 653,867). In MR analysis, genetic mimicry of serum FGF23 elevation was associated with increased CAVS risk [ORdiscovery = 3.081 (1.649–5.760), Pdiscovery = 4.21 × 10−4; ORreplication = 2.280 (1.461 – 3.558), Preplication = 2.82 × 10−4] without evidence of reverse causation (Psteiger= 7.21 × 10−98). Strong colocalisation association with CAVS was observed for FGF23 expression in the blood (PP.H4 = 0.96). Additionally, we identified some protein-protein interactions between FGF23 and known CAVS-associated genes. Serum calcium, phosphate, 25OH-VitD, and PTH failed to show causal effects on CAVS at Bonferroni-corrected significance (all P > 0.05/5 = 0.01). In conclusion, elevated serum FGF23 level may act as a causal risk factor for CAVS, and its mechanism of action in CAVS development may be independent of its function in regulating mineral metabolism. Hence, FGF23 may serve as a circulating marker and a promising preventive target for CAVS, warranting further investigation.
血清钙、磷酸盐、维生素 D、甲状旁腺激素和 FGF23 与主动脉狭窄风险的遗传关系
有报道称,钙化性主动脉瓣狭窄(CAVS)患者的矿物质代谢紊乱,包括血清钙、磷酸盐、25-羟维生素 D(25OH-VitD)、甲状旁腺激素(PTH)和成纤维细胞生长因子 23(FGF23)水平升高。然而,矿物质代谢在 CAVS 中的因果作用仍缺乏证据。在这项研究中,我们采用了一个系统的管道,结合孟德尔随机化(MR)、Steiger方向性检验、共定位分析、蛋白质-蛋白质网络和富集分析,来研究矿物质代谢对CAVS的因果效应。从大规模荟萃分析中提取了矿物质代谢标记物的全基因组关联研究(GWAS)和蛋白质定量性状位点数据。从作为发现队列和复制队列的两个独立 GWAS 数据集(n = 374 277 和 653 867)中获得了 CAVS 的汇总统计数据。在 MR 分析中,血清 FGF23 升高的遗传模拟与 CAVS 风险增加有关 [ORdiscovery = 3.081 (1.649-5.760),Pdiscovery = 4.21 × 10-4;ORreplication = 2.280 (1.461 - 3.558),Preplication = 2.82 × 10-4],但没有反向因果关系的证据(Psteiger= 7.21 × 10-98)。血液中 FGF23 的表达与 CAVS 有很强的共定位关联(PP.H4 = 0.96)。此外,我们还发现了 FGF23 与已知 CAVS 相关基因之间的一些蛋白质相互作用。血清钙、磷酸盐、25OH-VitD 和 PTH 未能显示出对 CAVS 的因果效应,但在 Bonferroni 校正后具有显著性(所有 P > 0.05/5 = 0.01)。总之,血清 FGF23 水平升高可能是 CAVS 的一个因果性风险因素,其在 CAVS 发生中的作用机制可能与其调节矿物质代谢的功能无关。因此,FGF23可作为一种循环标志物和有希望成为CAVS的预防靶点,值得进一步研究。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


