Impact of Warm Ischemia Time on Donation After Circulatory Death Kidney Transplant Outcomes
Abstract
Background
Efforts to address the shortage of donor organs include increasing the use of renal allografts from donors after circulatory death (DCD). While warm ischemia time (WIT) is thought to be an important factor in DCD kidney evaluation, few studies have compared the relationship between WIT and DCD kidney outcomes, and WIT acceptance practices remain variable.
Methods
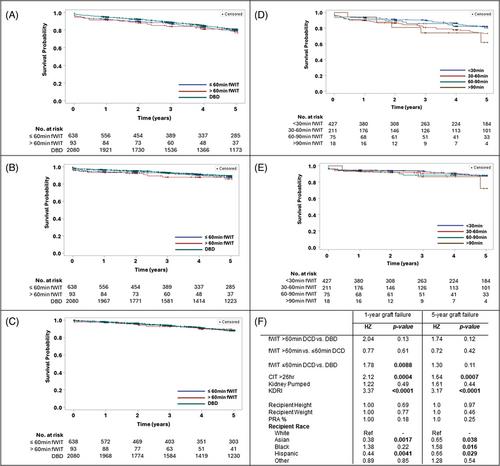
We conducted a single-center retrospective review of all adult patients who underwent deceased donor kidney transplantation from 2000 to 2021. We evaluated the impact of varied functional warm ischemia time (fWIT) in controlled DCD donors by comparing donor and recipient characteristics and posttransplant outcomes between high fWIT (>60 min), low fWIT (≤60 min), and kidneys transplanted from donors after brain death (DBD).
Results
Two thousand eight hundred eleven patients were identified, 638 received low fWIT DCD, 93 received high fWIT DCD, and 2080 received DBD kidneys. There was no significant difference in 5-year graft survival between the DCD low fWIT, high fWIT, and DBD groups, with 84%, 83%, and 83% of grafts functioning, respectively. Five-year patient survival was 91% in the low fWIT group, 92% in the high fWIT group, and 90% in the DBD group. An increase in kidney donor risk index (KDRI) (HR 3.37, 95% CI = 2.1–5.7) and high CIT compared to low CIT (HR 2.12, 95% CI = 1.4–3.1) have higher hazard ratios for 1-year graft failure.
Conclusions
Increased acceptance of kidneys from selected DCD donors with prolonged fWIT may present an opportunity to increase kidney utilization while preserving outcomes. Our group specifically prioritizes the use of kidneys from younger donors, with lower KDPI, and without acute kidney injury, or risk factors for underlying chronic kidney disease.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


