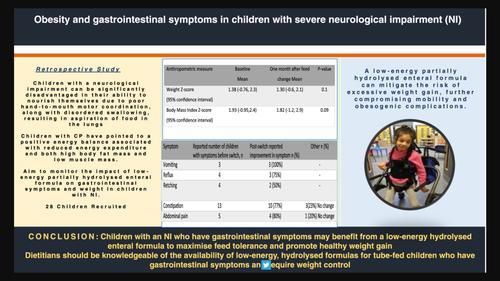
The impact of low-energy, partially hydrolysed enteral formula on gastrointestinal symptoms and weight in children with neurological impairment: a multicentre retrospective study
Abstract
Background
Neurological impairment (NI) relates to disorders of the central nervous system. The specific aetiology of NI varies but includes genetic, congenital abnormalities or brain injury. In children with severe NI, feeding impairments can lead to undernutrition, and some children require a feeding tube. Although tube feeding improves overall nutritional status, it has also been associated with excess body fat. Commercially available enteral formulas that are low in energy, hydrolysed and nutritionally adequate for protein and micronutrients are available to mitigate gastrointestinal symptoms and obesity.
Methods
This is a retrospective multicentre study of children who attended NI clinics between January 2022 and July 2023. Data were collected before and 1 month after receiving a low-energy, partially hydrolysed enteral formula (0.6 kcal/mL) on demographic data (age, sex, ethnicity and NI diagnosis), anthropometric measurements (weight, height, weight-for-age Z-score, height-for-age Z-score, body mass index [BMI] Z-score) and feed regimen (feed volume, total fluids and type of formula/supplements).
Results
Dietitians collected data on 28 children, the median age was 7 years (interquartile range [IQR] 3, 8). The most frequently recorded NI was cerebral palsy, in 13 of 28 children (48%). Before the formula switch, the most frequently reported gastrointestinal symptom was constipation, in 13 of 28 children. Within 1 month of switching to a low-energy, hydrolysed formula, 10 of the 13 (77%) children reported an improvement in constipation. Before the formula switch, all 28 children were experiencing excessive weight gain. After the formula was switched to low-energy, hydrolysed formula, dietitians reported that 20 of the 28 (76%) children's weight either stabilised or reduced after 1 month. There was no statistically significant difference in weight-for-age Z-score or BMI Z-scores postswitch of formula (p-value 0.1 and 0.09, respectively). Fibre intake increased significantly from 3.3 to 8.1 g/day (p-value < 0.01) after formula switch. The number of children whose feed regimens were simplified after switching to a low-energy, partially hydrolysed formula was 24 of 28 (91%).
Conclusions
Children with an NI who have gastrointestinal symptoms may benefit from a low-energy, hydrolysed enteral formula to maximise feed tolerance and promote healthy weight gain. In addition, changing to a low-energy, hydrolysed formula may simplify feed regimens by eliminating the need for additional electrolytes, multivitamins and fluid boluses. Healthcare professionals should be knowledgeable about the effectiveness and availability of a low-energy, hydrolysed formula.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


