Kaifeng Jin, Jingtong Xu, Xiaohe Su, Ziyue Xu, Bingyu Li, Ge Liu, Hailong Liu, Yiwei Wang, Yu Zhu, Le Xu, Weijuan Zhang, Zhaopei Liu, Zewei Wang, Yuan Chang, Jiejie Xu
下载PDF
{"title":"TP53 disruptive mutation predicts platinum-based chemotherapy and PD-1/PD-L1 blockade response in urothelial carcinoma","authors":"Kaifeng Jin, Jingtong Xu, Xiaohe Su, Ziyue Xu, Bingyu Li, Ge Liu, Hailong Liu, Yiwei Wang, Yu Zhu, Le Xu, Weijuan Zhang, Zhaopei Liu, Zewei Wang, Yuan Chang, Jiejie Xu","doi":"10.1002/path.6266","DOIUrl":null,"url":null,"abstract":"<p><i>TP53</i> mutation is one of the most common genetic alterations in urothelial carcinoma (UrCa), and heterogeneity of <i>TP53</i> mutants leads to heterogeneous clinical outcomes. This study aimed to investigate the clinical relevance of specific <i>TP53</i> mutations in UrCa. In this study, a total of eight cohorts were enrolled, along with matched clinical annotation. <i>TP53</i> mutations were classified as disruptive and nondisruptive according to the degree of disturbance of p53 protein function and structure. We evaluated the clinical significance of <i>TP53</i> mutations in our local datasets and publicly available datasets. The co-occurring events of <i>TP53</i> mutations in UrCa, along with their therapeutic indications, functional effects, and the tumor immune microenvironment, were also investigated. <i>TP53</i> mutations were identified in 49.7% of the UrCa patients. Within this group, 25.1% of patients carried <i>TP53</i><sup>Disruptive</sup> mutations, a genetic alteration correlated with a significantly poorer overall survival (OS) when compared to individuals with <i>TP53</i><sup>Nondisruptive</sup> mutations and those with wild-type <i>TP53</i>. Significantly, patients with <i>TP53</i><sup>Disruptive</sup> mutations exhibit an increased probability of responding favorably to PD-1/PD-L1 blockade and chemoimmunotherapy. Meanwhile, there was no noteworthy distinction in OS among patients with varying <i>TP53</i> mutation status who underwent chemotherapy. Samples with <i>TP53</i><sup>Disruptive</sup> mutations showed an enriched APOBEC- and POLE-related mutational signature, as well as an elevated tumor mutation burden. The sensitivity to immunotherapy in tumors carrying <i>TP53</i><sup>Disruptive</sup> mutation may be attributed to the inflamed tumor microenvironment characterized by increased CD8<sup>+</sup>T cell infiltration and interferon-gamma signaling activation. In conclusion, UrCa patients with <i>TP53</i><sup>Disruptive</sup> mutations have shown reduced survival rates, yet they may respond well to PD-1/PD-L1 blockade therapy and chemoimmunotherapy. By distinguishing specific <i>TP53</i> mutations, we can improve risk stratification and offer personalized genomics-guided therapy to UrCa patients. © 2024 The Authors. <i>The Journal of Pathology</i> published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.</p>","PeriodicalId":232,"journal":{"name":"The Journal of Pathology","volume":"263 2","pages":"139-149"},"PeriodicalIF":5.6000,"publicationDate":"2024-02-21","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://onlinelibrary.wiley.com/doi/epdf/10.1002/path.6266","citationCount":"0","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"The Journal of Pathology","FirstCategoryId":"3","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/path.6266","RegionNum":2,"RegionCategory":"医学","ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q1","JCRName":"ONCOLOGY","Score":null,"Total":0}
引用次数: 0
引用
批量引用
Abstract
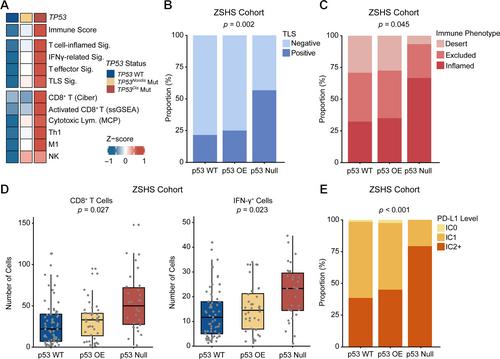
TP53 mutation is one of the most common genetic alterations in urothelial carcinoma (UrCa), and heterogeneity of TP53 mutants leads to heterogeneous clinical outcomes. This study aimed to investigate the clinical relevance of specific TP53 mutations in UrCa. In this study, a total of eight cohorts were enrolled, along with matched clinical annotation. TP53 mutations were classified as disruptive and nondisruptive according to the degree of disturbance of p53 protein function and structure. We evaluated the clinical significance of TP53 mutations in our local datasets and publicly available datasets. The co-occurring events of TP53 mutations in UrCa, along with their therapeutic indications, functional effects, and the tumor immune microenvironment, were also investigated. TP53 mutations were identified in 49.7% of the UrCa patients. Within this group, 25.1% of patients carried TP53 Disruptive mutations, a genetic alteration correlated with a significantly poorer overall survival (OS) when compared to individuals with TP53 Nondisruptive mutations and those with wild-type TP53 . Significantly, patients with TP53 Disruptive mutations exhibit an increased probability of responding favorably to PD-1/PD-L1 blockade and chemoimmunotherapy. Meanwhile, there was no noteworthy distinction in OS among patients with varying TP53 mutation status who underwent chemotherapy. Samples with TP53 Disruptive mutations showed an enriched APOBEC- and POLE-related mutational signature, as well as an elevated tumor mutation burden. The sensitivity to immunotherapy in tumors carrying TP53 Disruptive mutation may be attributed to the inflamed tumor microenvironment characterized by increased CD8+ T cell infiltration and interferon-gamma signaling activation. In conclusion, UrCa patients with TP53 Disruptive mutations have shown reduced survival rates, yet they may respond well to PD-1/PD-L1 blockade therapy and chemoimmunotherapy. By distinguishing specific TP53 mutations, we can improve risk stratification and offer personalized genomics-guided therapy to UrCa patients. © 2024 The Authors. The Journal of Pathology published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.
TP53破坏性突变可预测铂类化疗和PD-1/PD-L1阻断剂对尿路上皮癌的反应。
TP53突变是尿路上皮癌(UrCa)最常见的基因改变之一,TP53突变体的异质性导致了不同的临床结果。本研究旨在探讨特定TP53突变在尿路癌中的临床意义。本研究共纳入了八个队列,并进行了匹配的临床注释。根据p53蛋白功能和结构的紊乱程度,TP53突变被分为破坏性和非破坏性突变。我们评估了本地数据集和公开数据集中 TP53 突变的临床意义。我们还研究了TP53突变在UrCa中的并发症及其治疗适应症、功能效应和肿瘤免疫微环境。49.7%的UrCa患者发现了TP53突变。在这一群体中,25.1%的患者携带TP53破坏性突变,与TP53非破坏性突变和野生型TP53患者相比,这种基因改变与较差的总生存期(OS)相关。值得注意的是,TP53Disruptive突变患者对PD-1/PD-L1阻断和化疗免疫疗法产生良好反应的概率增加。同时,在接受化疗的不同TP53突变状态的患者中,OS没有明显的区别。具有TP53破坏性突变的样本显示出丰富的APOBEC和POLE相关突变特征,以及较高的肿瘤突变负荷。携带 TP53Disruptive 突变的肿瘤对免疫疗法的敏感性可能归因于以 CD8+ T 细胞浸润增加和干扰素-γ 信号激活为特征的炎症肿瘤微环境。总之,具有 TP53Disruptive 突变的 UrCa 患者生存率降低,但他们可能对 PD-1/PD-L1 阻断疗法和化学免疫疗法反应良好。通过区分特定的TP53突变,我们可以改善风险分层,并为UrCa患者提供个性化的基因组指导治疗。© 2024 作者。病理学杂志》由 John Wiley & Sons Ltd 代表大不列颠及爱尔兰病理学会出版。
本文章由计算机程序翻译,如有差异,请以英文原文为准。

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


